Paralysis is a vast topic in human medicine. Primarily, paralysis is described as the impairment or loss of involuntary muscular movement in any part of the body, especially the four limbs. In normal humans, uninjured nerve fibers in the body send signals from the voluntary muscles to the brain.
Paralysis occurs when your voluntary muscles cannot respond to corresponding movements. In direct response, the voluntary muscles may initiate movements and sudden jerks. The response triggered largely depends on the location of the muscle.
These lost sensations, in this case, may be touch, sore pressures, warmth, or tickles. People that have a disease or pathological condition affecting how nerves send signals or how these signals are interpreted may develop paralysis.
Depending on the underlying cause and the severity of nerve damage caused to the central nervous system, paralysis may be described as
- a) Partial
- b) Complete
- c) Localized
- d) Generalized
- e) Permanent
- f) Temporary
In a 2013 estimate, research suggests that nearly 5.4 million people live with paralysis in the United States (Armour et al., 2016).
This article describes two of the most researched types of paralysis in humans; Paraplegia and Tetraplegia.
Tetraplegia Vs Paraplegia
Paraplegia and Tetraplegia are two severe forms of paralysis commonly linked with brain and spinal cord injury. In Tetraplegia, also known as Quadriplegia, both the arms and legs are paralyzed. In many cases, tetraplegia occurs due to a congenital condition or an illness.
Your healthcare provider may use the term ‘Paraparesis’ to describe Paraplegia. In this form of paralysis, both legs and the lower body are paralyzed, resulting in walking difficulties and frequent urinary tract infections in many patients.
Paraplegia is complex and further categorized into three different types;
- Hereditary Spastic Paraplegia (HSP)
This is paraplegia linked with a hereditary factor. According to the National Institute of Neurological Disorders and Stroke, HSP refers to ‘a group of inherited disorders characterized by progressive paralysis of the legs.’ In the early stages of this paralysis, people with this condition may present stiffness and mild gait difficulties (Blackstone et al., 2018).
- Complete Paraplegia
People with complete paraplegia have no voluntary command over the leg muscles, and feelings of tough and sore pressure are also entirely lost. The symptoms that might likely develop include generalized weakness, inability to walk, and loss of bladder and bowel function.
- Incomplete or Partial Paraplegia (Paraparesis)
In a few cases, paraplegia might not affect both legs. One leg may be fully paralyzed, irresponsive to nerve signals from the brain, and incapable of voluntary movements. The other may have limited functionality. This condition is described as incomplete paraplegia.
Other severe forms of paralysis include;
- Triplegia
This is a paralysis condition characterized by loss of movement in both legs and one arm.
- Quadriparesis
In this type of paralysis, there is temporary or permanent paralysis of the four limbs.
- Monoplegia
This happens when a stroke or a neurological disease causes paralysis affecting just one limb, usually an arm.
- Hemiplegia
This condition describes paralysis on one side of the body caused by brain and spinal cord injuries.
Causes and Pathophysiology
- Spinal Cord Injury
Spinal cord injuries are serious health conditions occurring when the axons of nerves of the spinal cord are injured, damaged, or disrupted. This leads to loss of sensory and motor functions below the injury site.
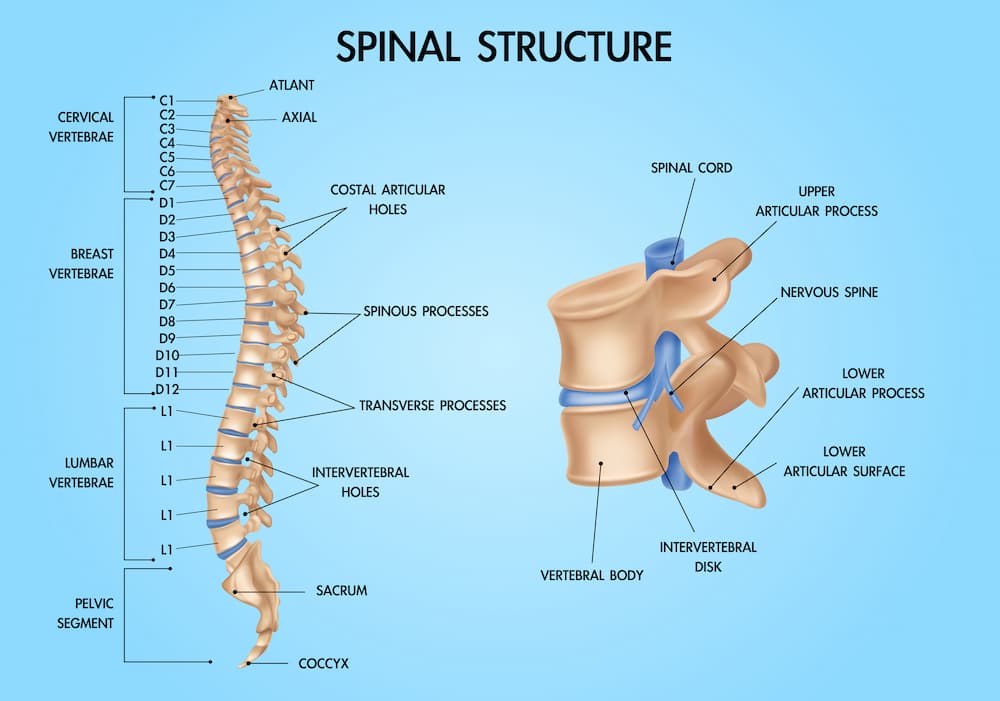
Structurally, the spinal column houses the spinal cord -a tube-like bundle of nerve fibers and cells conveying neural signals from the brain to the body and vice versa. The spinal column bones -the vertebras- protect the cord from injury.
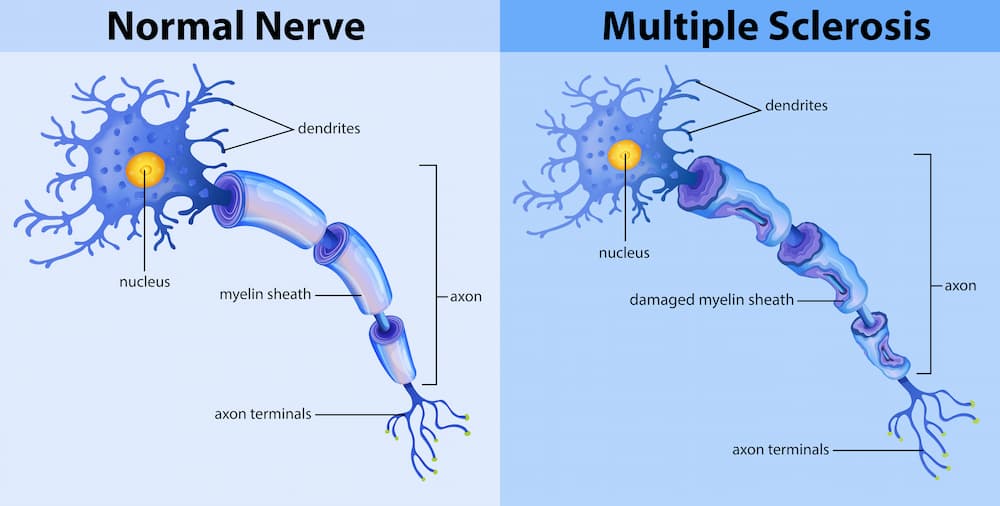
Dislocations and structural damages to the vertebras can leave a section of the spinal cord exposed and vulnerable to injuries. Primary injuries on the cord can cause an inflammation of the myelin sheath –an insulating layer of protein and fatty substances covering the nerve fibers.
Spinal cord injuries that cause paralysis are mainly due to trauma and brute force. Inflammation and subsequent damage to the sheath slow down sensory perception from the spinal cord, causing paralysis in a different part of the body. Common non-traumatic causes of spinal injuries include cancer, neurological disorders, arthritis, and spinal disk degeneration.
In adult humans, the spinal cords are complex structures divided into several regions;
- The Cervical spine is found in the neck region and is numbered C1 – C7
- The Thoracic spine is found in the upper back region and is numbered T1 – T12
- The Lumbar spine is found near the base of the spine and is numbered L1 – L5
- The Sacral spine is found at the very end of the spinal column and is numbered S1 – S5
The nature and severity of paralysis depending on the region of the spinal cord where it occurs. Tetraplegia is caused by injury to the spinal nerve fibers found in the C1 – C8 region. On the other hand, Paraplegia is caused by spinal cord injuries in the thoracic vertebra (T1 – T12), lumbar vertebra (L1 – L5), or sacral vertebra (S1 – S5) (Chin et al., 2017).
- Stroke
In 2013 research published by the American Journal of Public Health, stroke was a leading cause of paralysis, linked to about 33.7% percent of all reported cases (Armour et al., 2016). It is a neurological disorder characterized by the blockage of blood vessels or the bursting of blood vessels. In either case, the disruption in normal blood flow triggers the formation of clots.
In ischemic stroke (87%of all stroke cases), blood clots block the small vessels and cut off the oxygen supply to the brain (Kuriakose et al., 2020). With a limited supply of oxygen, brain cells begin to die, causing an alteration in the generation and transfer of neuronal signals to the other parts of the body. This ultimately leads to paralysis.
In most cases, paralysis occurs on the opposite side of the body where the brain injury had occurred. This is because each side of the brain controls neuronal signals and movement on the opposite side of the body. So, if a stroke occurs in the brain’s left hemisphere, paralysis may occur on the right side of the body.
- Multiple Sclerosis (MS)
MS is a chronic inflammatory disease that causes spinal cord lesions and inflammation of the spinal cord’s myelin sheath. The leading causes of MS in people remain unclear. However, the available evidence suggests a complex interplay of genetic and environmental factors. Smoking, vitamin deficiencies, and exposure to infectious agents have also been implicated (Ghasemi et al., 2017).
Inflammation of the myelin sheath slows down the speed of neuronal signals along the spinal cord. Once signal conduction is affected, the brain exerts limited or no control on voluntary muscle movements, causing paralysis. The type of paralysis depends on the severity of nerve damage.
Spinal lesions also limit signal transfer along the spinal cord, causing chronic pain, loss of coordination, muscle spasms, and prickling sensation in some people. MS can cause both paraplegia and tetraplegia, depending on the severity of the condition.
- Neurodegenerative Diseases
Neurodegenerative diseases are age-dependent health conditions primarily affecting neurons. The most common diagnoses once include Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, and amyotrophic lateral sclerosis. The pathological features of these conditions in the progressive death of neuron cells (Verkhratsky et al., 2017).
Neuronal cell death negatively affects the brain and spinal cord and alters the brain’s primary functions. The death of neuron cells due to brain injury and spinal cord injury directly affects signals transmitted to the rest of the body. This can cause both tetraplegia and paraplegia and other types of paralysis.
Diagnosis of Paraplegia and Tetraplegia
The diagnosis of paraplegia and tetraplegia involve a clinical examination to understand the nature of the paralysis and locate where the injury occurred. A computer tomography (CT) may be conducted to pinpoint injuries to the spinal columns. Magnetic resonance imaging can show the nature and extent of damage to the spinal cord.
Spinal lesions can also be examined using magnetic resonance imaging. Sometimes, your doctor may order blood tests to scan for nutritional deficiencies, assess the risk of stroke, and understand the extent of brain injury. Electromyography (EMG) tests may also be used to read electrical exchanges that determine the brain’s function.
Your doctor may combine two or more of these tests before making a confirmed diagnosis.
Treatment of Paraplegia and Tetraplegia
Currently, there is no cure for both paraplegia and tetraplegia. The focus is on managing pain and other symptoms and reducing the risk of long-term complications.
These treatments also focus on;
- Reducing inflammation of the myelin sheath
- Improving the rate of nerve impulse transfer
- Managing any complications
- Improving a person’s life quality
The therapy options available for people with these paralysis conditions include;
- Medications
- Baclofen
Your doctor may prescribe baclofen -a first-line centrally-acting drug to treat paralysis in adults. Once administered orally in appropriate doses, this medication crosses the blood-brain barrier and becomes rapidly absorbed. Research suggests baclofen improves muscle movement in the limbs and also reduces the rate of muscle deterioration (Thomas et al., 2010).
- Corticosteroids
Corticosteroids like hydrocortisone and prednisone may be prescribed to reduce the inflammation of the myelin sheath. This systemic action of corticosteroids limits damage to the healthy spinal nerve in partial paralysis and may terminate the course of disease progression (Ramsey et al., 2000). If you tolerate these medications properly, your doctor may increase the dosage with time and monitor you for some expected clinical improvements.
- Blood thinners and Antibiotics
Peer-reviewed studies recommend antibiotics and blood thinners such as clopidogrel and aspirin to manage paralysis in older people. Antibiotics lower the risk of infections, ensuring the inflamed nerve fibers are not infected (Hurkacz et al., 2021). Combining blood thinners and antibiotics may help improve the symptoms of both paraplegia and tetraplegia.
- Surgical Procedures
Paralysis and reconstructive nerve surgical procedures are becoming increasingly popular. Your doctor may prescribe this as emergency surgery to treat paralysis. Surgical options might be considered if you develop complications or experience chronic, long-term pain.
Surgical recommendations depend on the type and severity of paralysis. However, these procedures are performed to reduce the symptoms of paralysis directly. They influence the central nervous system and manage the primary causes of nerve signal block.
Surgical procedures may also remove tumors on the spinal cord, align a dislocated vertebra, repair busted arteries, and correct spinal cord inflammation.
- Spinal Cord Injury Rehabilitation
Physical and psychological therapy are essential parts of the recovery step for people with paralysis. In managing stroke and other leading causes of paralysis, spinal cord rehabilitation help reduce the risk of obesity, pressure sores, diabetes, and other complications of acute loss of mobility.
Physiologists recommend that patients pursue physical therapy to improve muscle functions. As a supporting recommendation, people with paraplegia or tetraplegia are expected to be engaged in at least 20 minutes of tolerated aerobic activity per day (Buchholz et al., 2009).
Additional aerobic activity, including swimming, walking, and wheelchair mobility, has significantly improved aerobic conditioning and muscle retention (Eng et al., 2007).
Conclusion
Loss of muscle control can negatively impact a person’s quality of life. While paraplegia refers to the loss of muscle control in both legs, tetraplegia affects the limbs causing partial or complete paralysis.
In people with these conditions, the challenges posed by immobility are enormous, making them vulnerable to other medical conditions, including deep venous thrombosis. Early diagnosis and management are considered the best approach to improving the prognosis of these conditions. In older patients, routine examination of nerve coordination and muscle health is advised.
Although both conditions are not curable, partial or complete control of the affected regions may be achieved with a suitable therapy plan.
References
- Chin LS, Mesfin FB, Dawodu ST. Spinal cord injuries: Practice essentials, background, anatomy, pathophysiology, etiology, epidemiology, prognosis, patient education. [Internet] 12 July 2022. Available from: http://www.emedicine.com/pmr/topic182.htm.
- Armour BS, Courtney-Long EA, Fox MH, Fredine H, Cahill A. Prevalence and Causes of Paralysis-United States, 2013. Am J Public Health. 2016 Oct;106(10):1855-7
- Kuriakose D, Xiao Z. Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives. Int J Mol Sci. 2020 Oct 15;21(20):7609.
- Ghasemi N, Razavi S, Nikzad E. Multiple Sclerosis: Pathogenesis, Symptoms, Diagnoses and Cell-Based Therapy. Cell J. 2017 Apr-Jun;19(1):1-10
- Verkhratsky A, Zorec R, Rodriguez JJ, Parpura V. Neuroglia: Functional Paralysis and Reactivity in Alzheimer’s Disease and Other Neurodegenerative Pathologies. Adv Neurobiol. 2017; 15:427-449.
- Thomas CK, Häger-Ross CK, Klein CS. Effects of baclofen on motor units paralyzed by chronic cervical spinal cord injury. Brain. 2010 Jan;133(Pt 1):117-25
- Ramsey MJ, DerSimonian R, Hotel MR, Burgess LP. Corticosteroid treatment for idiopathic facial nerve paralysis: a meta-analysis. Laryngoscope. 2000 Mar;110(3 Pt 1):335-41.
- Hurkacz M, Dobrek L, Wiela-Hojeńska A. Antibiotics and the Nerves-Which Face of Antibiotic Therapy Is Real, Dr. Jekyll (Neurotoxicity) or Mr. Hyde (Neuroprotection)? Molecules. 2021 Dec 9;26(24):7456.
- Buchholz AC, Martin Ginis KA, Bray SR, Craven BC, Hicks AL, Hayes KC, Latimer AE, McColl MA, Potter PJ, Wolfe DL. Greater daily leisure time physical activity is associated with lower chronic disease risk in adults with spinal cord injury. Appl Physiol Nutr Metab. 2009 Aug;34(4):640-7.
- Eng JJ, Teasell R, Miller WC, Wolfe DL, Townson AF, Aubut JA, Abramson C, Hsieh JT, Connolly S, Konnyu K; the SCIRE Research Team. Spinal Cord Injury Rehabilitation Evidence: Methods of the SCIRE Systematic Review. Top Spinal Cord Inj Rehabil. 2007 Summer;13(1):1-10.
- Blackstone C. Hereditary spastic paraplegia. Handb Clin Neurol. 2018;148:633-652.